Нутритивная поддержка
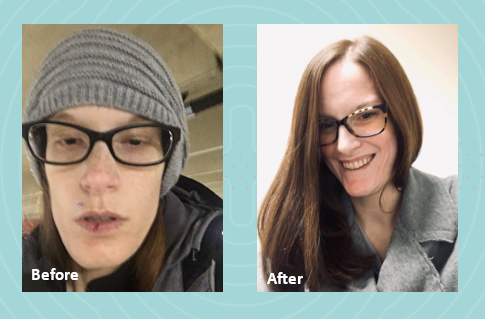
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

Нутритивная поддержка
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
Другое
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
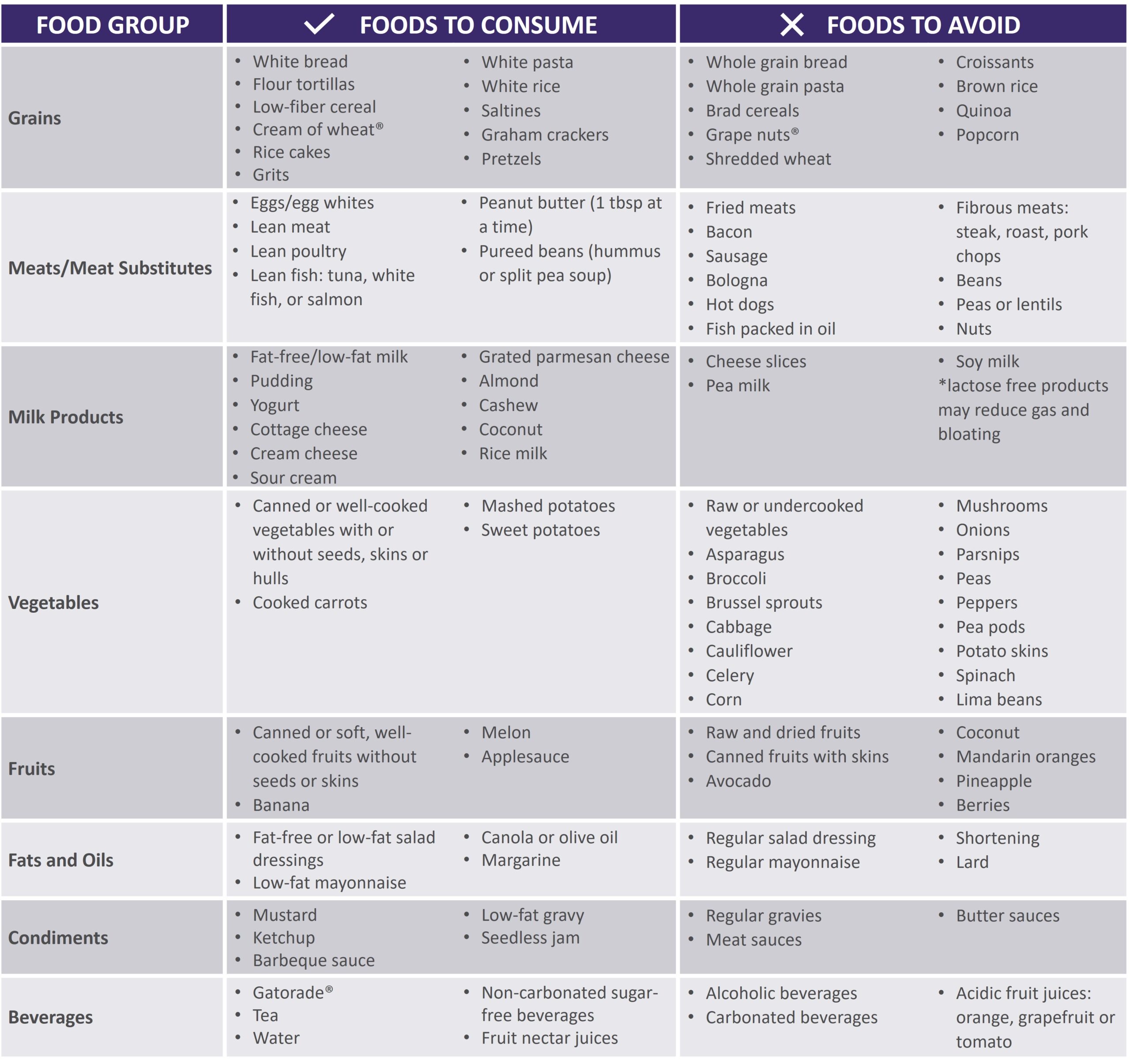
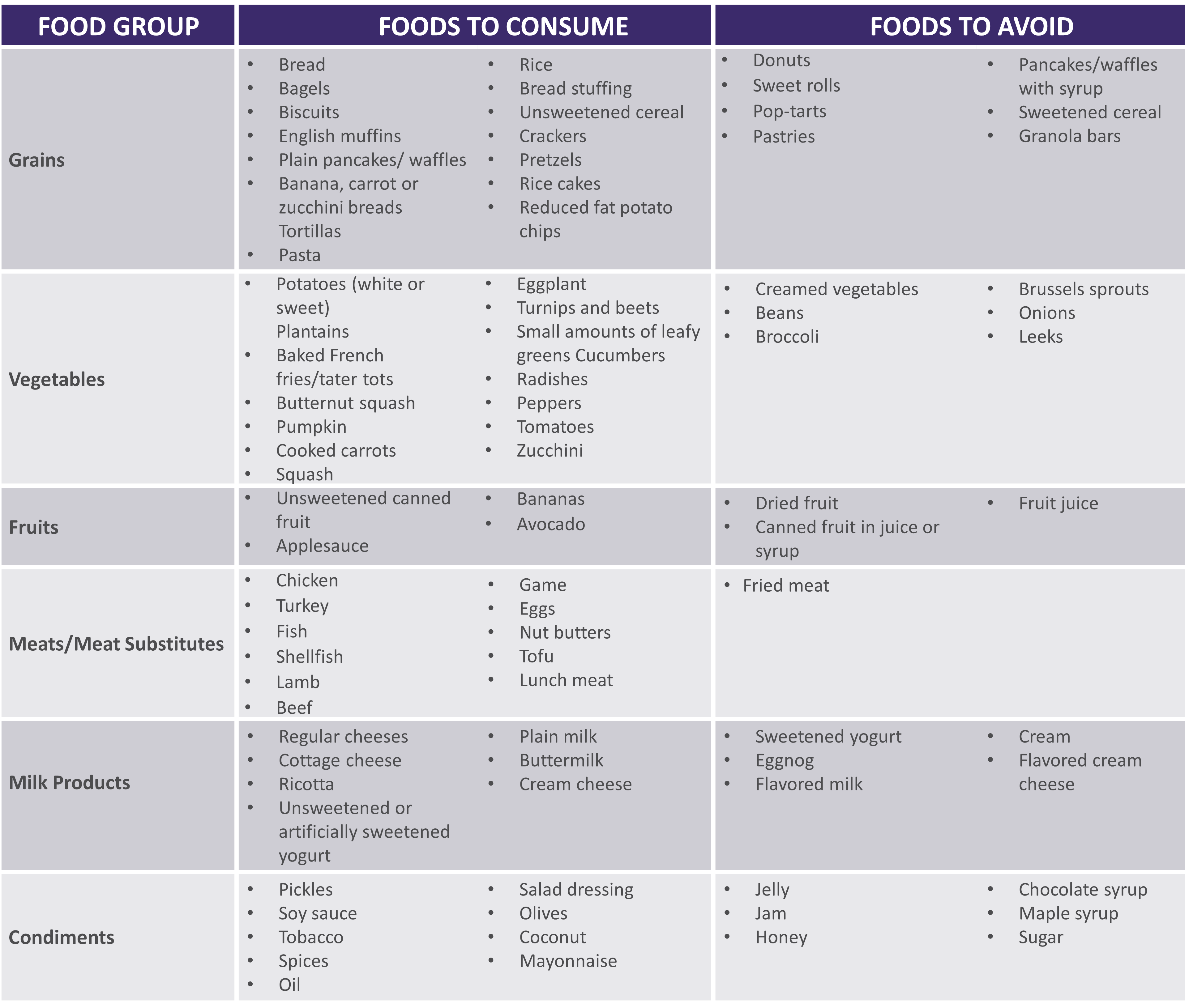
See below for help in choosing more optimal foods from each food group:
 |
|
Gastroparesis Sample Menus |
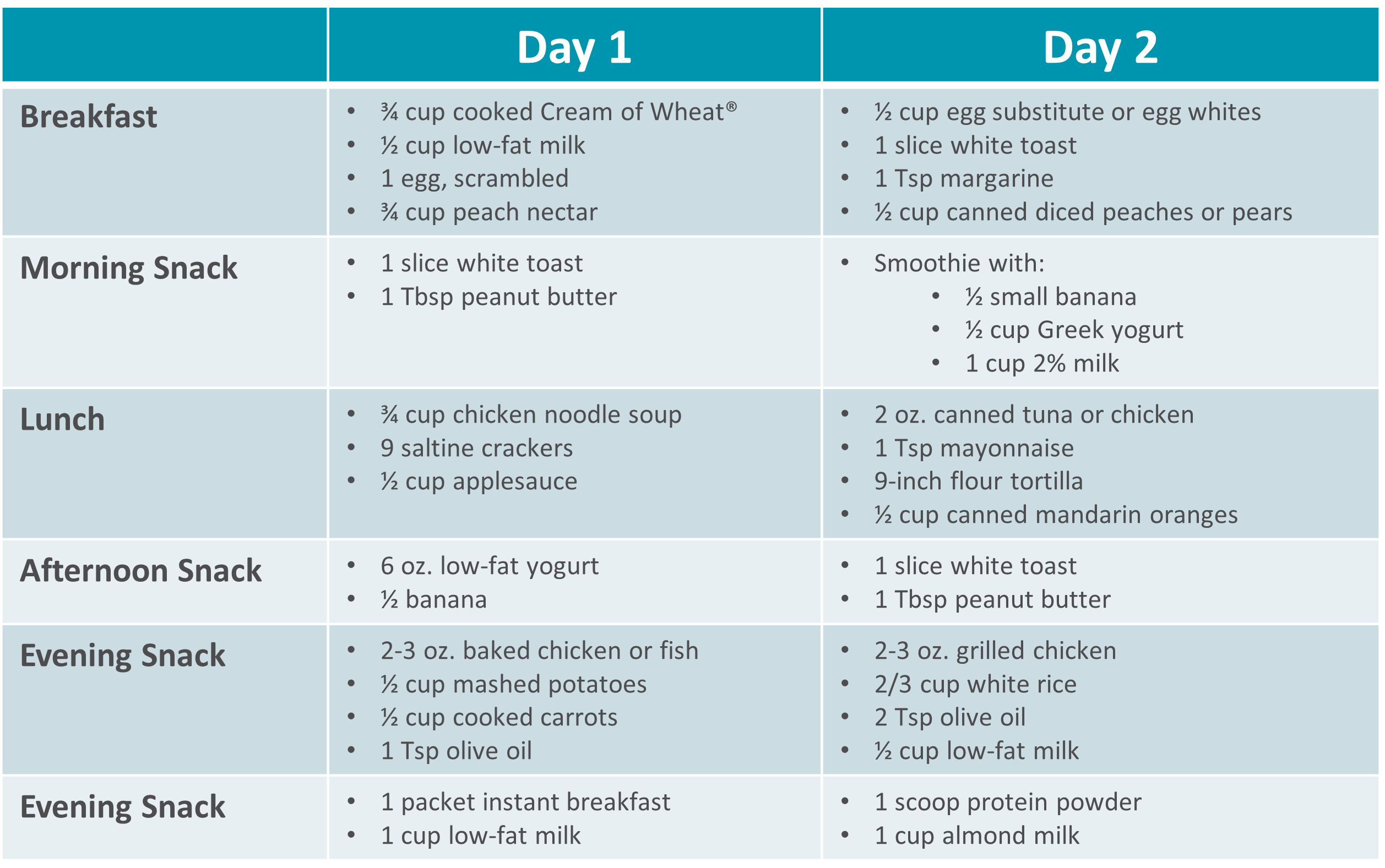 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Нутритивная поддержка
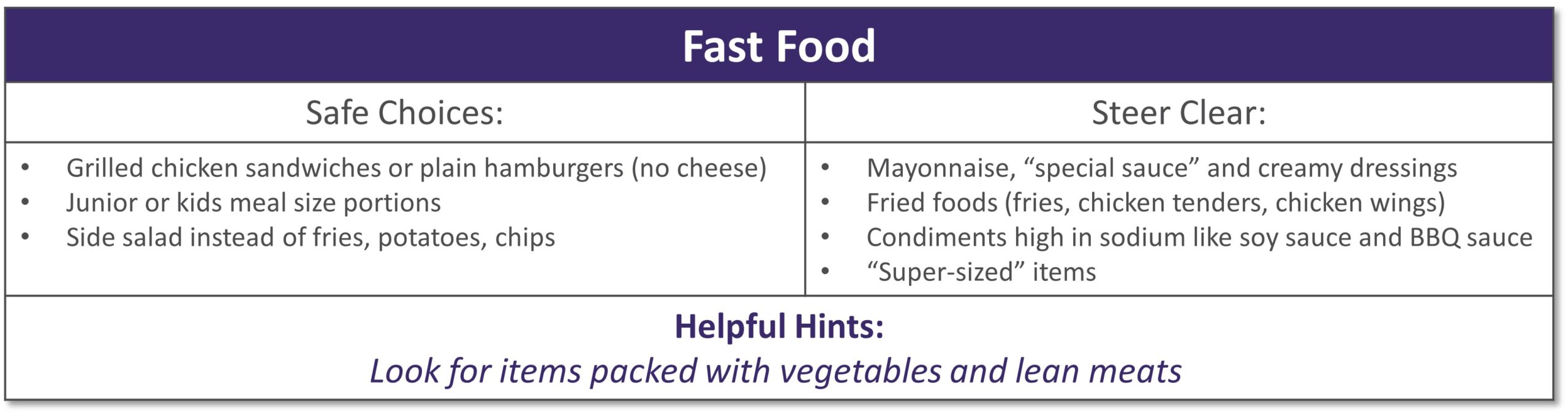
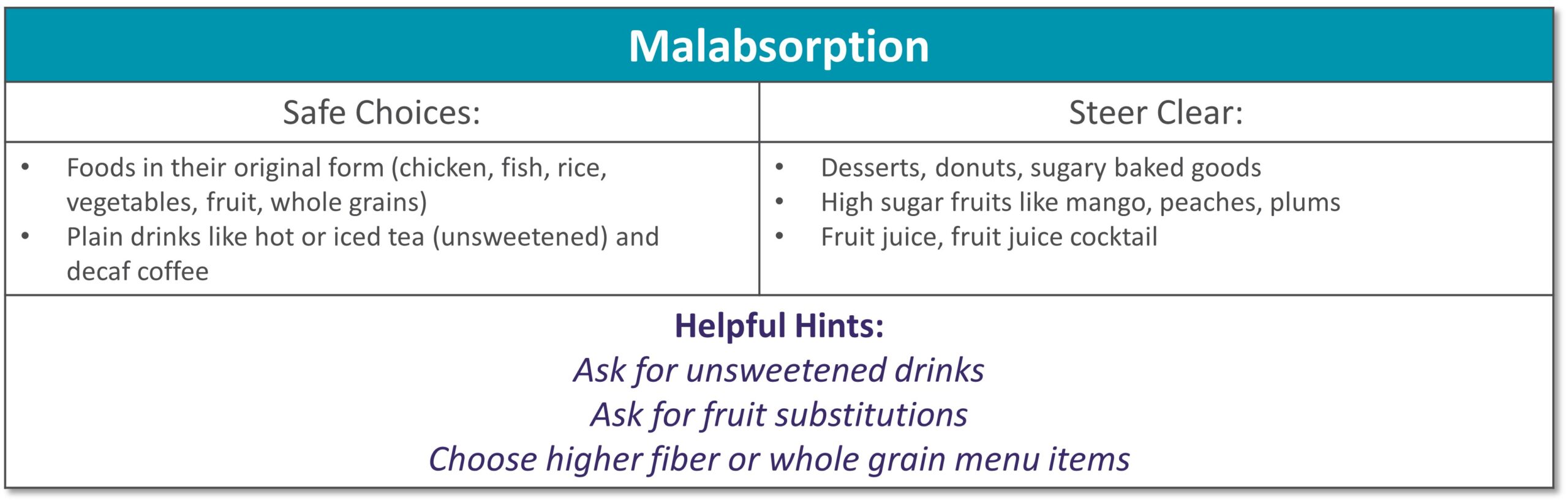
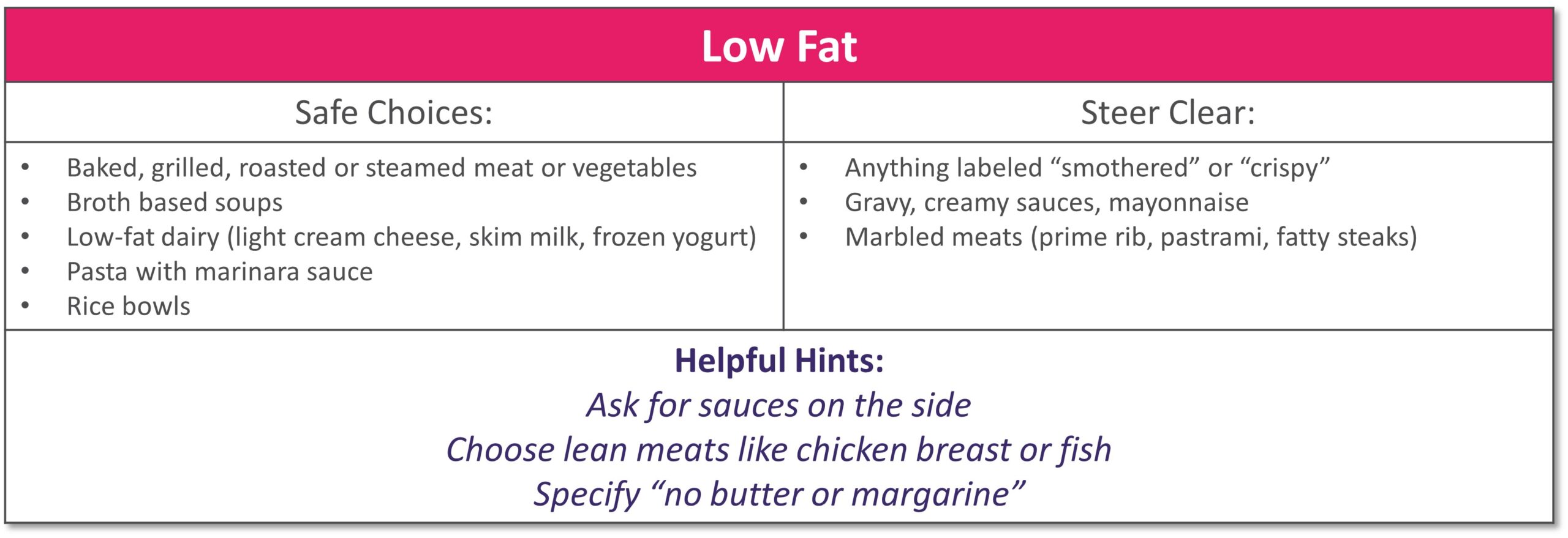
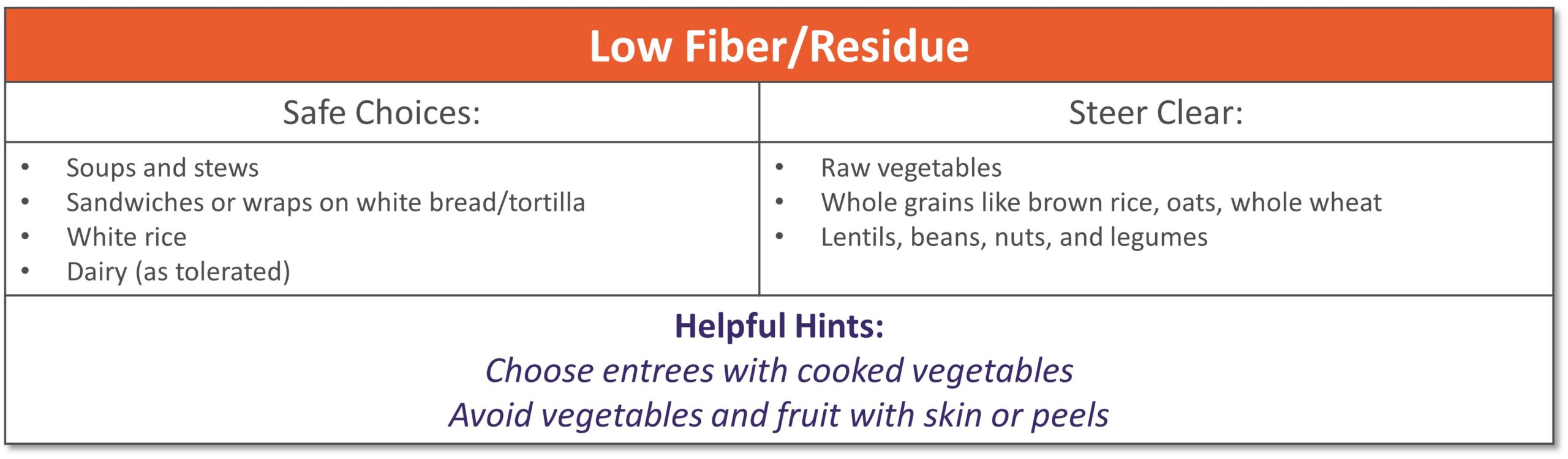
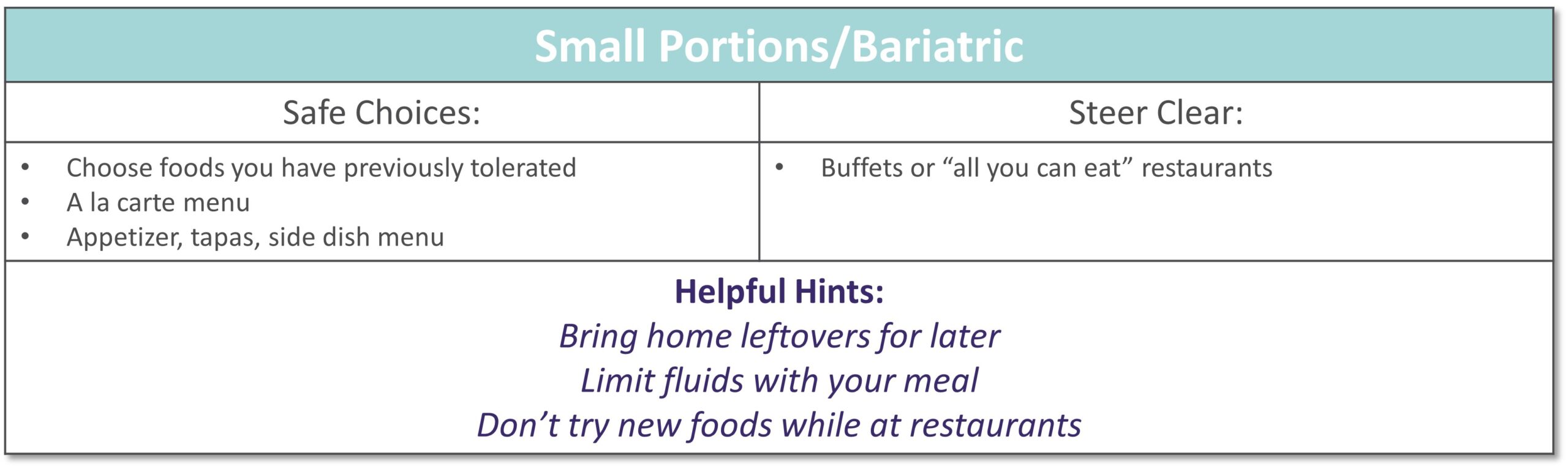
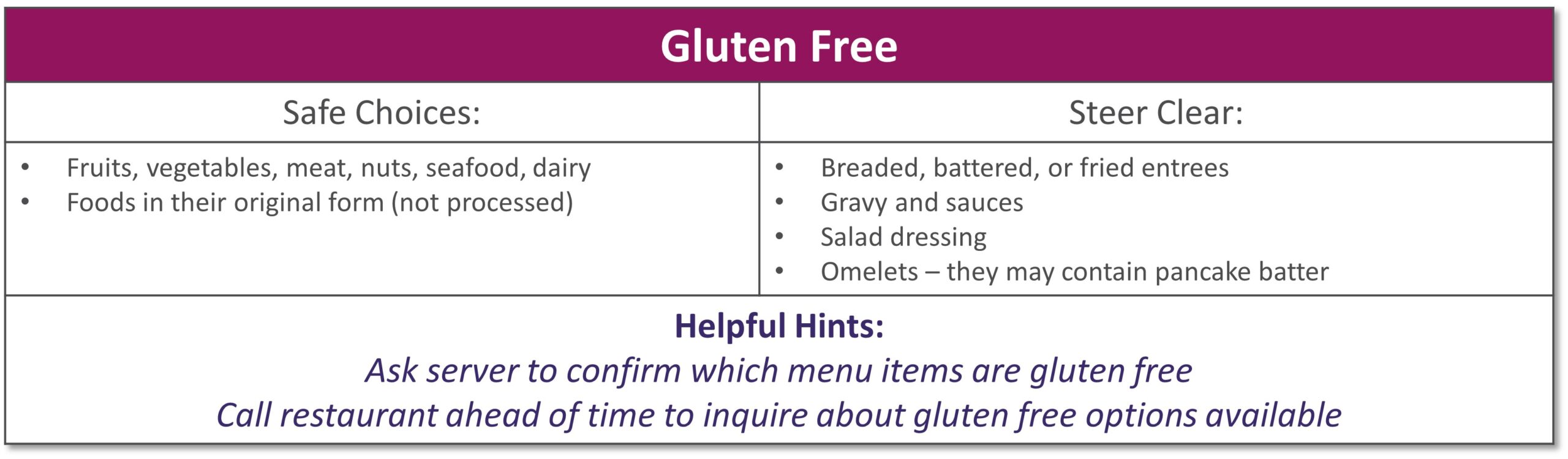
Dining out at restaurants is a nice treat but also challenging when trying to stick with your therapeutic diet, especially with gastrointestinal diseases. Most restaurants have menus and nutritional information available online. Restaurants are not required to have nutrition information available if they have less than 20 locations. Follow these tips to navigate eating out if you have specialized nutrition needs.
GENERAL TIPS:
- Research the menu online
- Pick a cuisine you tolerate
- Ask server for nutritional information or ingredients if not listed on the menu
- Do NOT be afraid to ask to customize the meal or ask for specific changes
- Communicate with wait staff if you have a food allergy or intolerance
- HAVE A PLAN AND STICK WITH IT!
|
|
|
|
|
|
|
|
|
|
|
|
|
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health. *This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information. |

Нутритивная поддержка
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
- Fluids
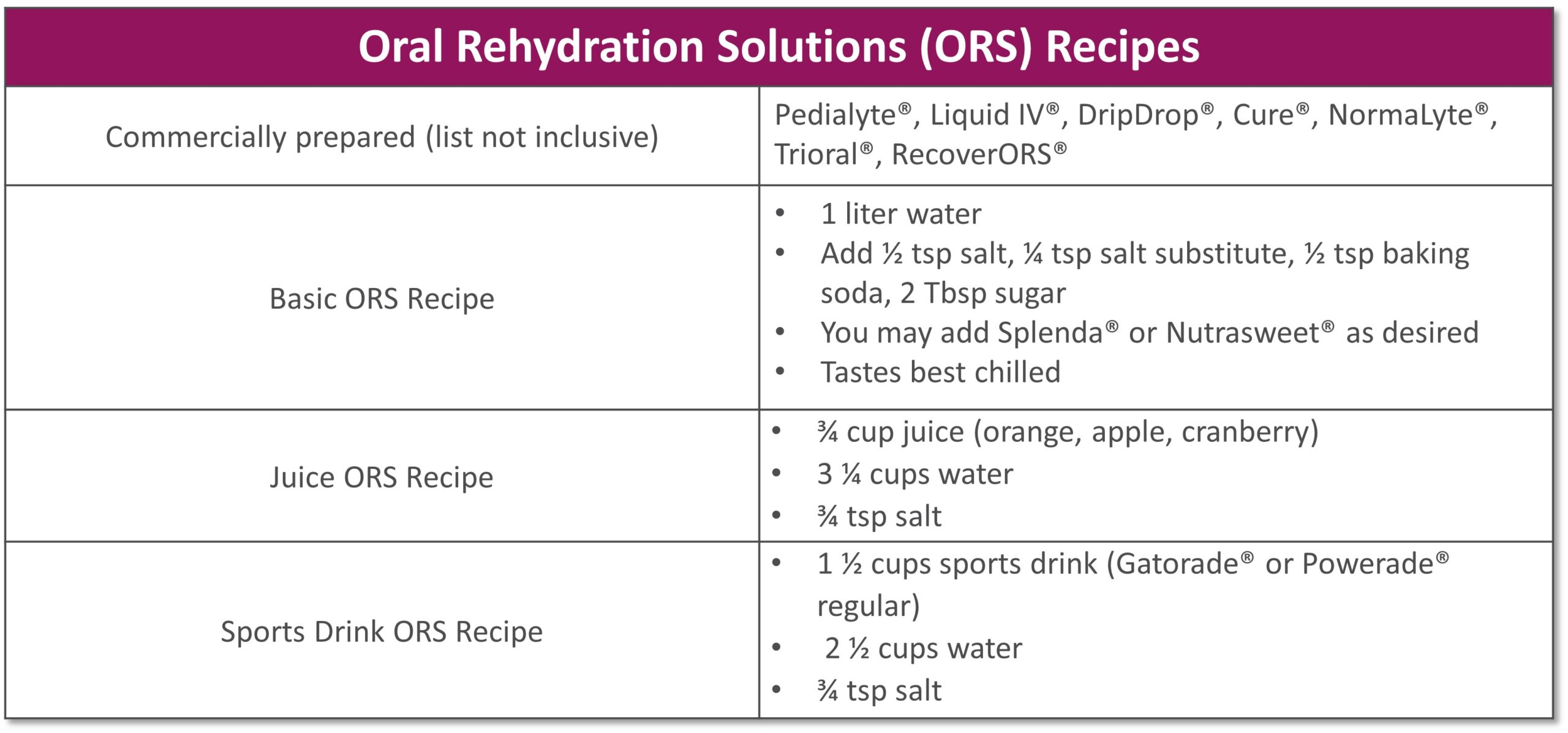
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- Другое
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
SBS Sample Menu |
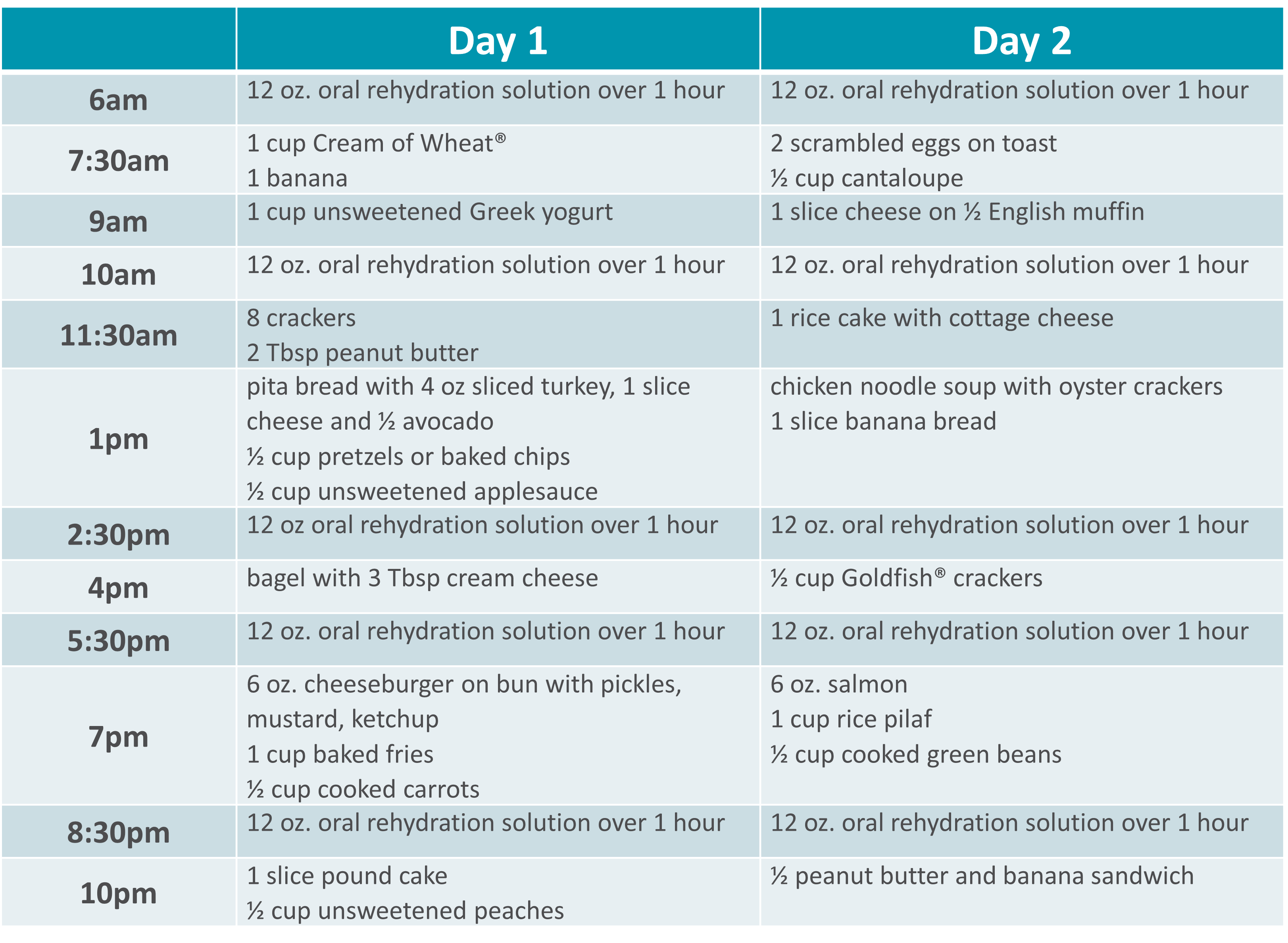 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Нутритивная поддержка
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
*Неделя повышения осведомленности об истощении™ — торговый знак Американского общества парентерального и энтерального питания (ASPEN). Используется с разрешения ASPEN.

Нутритивная поддержка
 Лечебное питание — это результат усилий нескольких специалистов.
Лечебное питание — это результат усилий нескольких специалистов.
Сертифицированные диетологи Option Care Health являются важной частью команды специалистов, занимающихся нутритивной поддержкой. Они взаимодействуют с медсестрами, фармацевтами и другим лечащим персоналом предоставления нашим пациентам самой высококачественной медицинской помощи как в больнице, так и на дому.
Мы ориентируемся на совместное сотрудничество, так как знаем, что такой подход наиболее эффективен для пациентов и способствует достижению оптимальных результатов.
Нажмите на ссылку ниже, чтобы прочитать статью, опубликованную в Today’s Dietitian.

Нутритивная поддержка
After overcoming ovarian cancer in 1995, retired nurse Lydia Zwilling found herself facing an arduous battle to reclaim her health. Nearly a quarter million women are diagnosed with ovarian cancer every year and for most, treatment goes according to plan. Unfortunately, some like Lydia, experience complications that last a lifetime.
While radiation therapy may have saved Lydia’s life, it also burned her small intestine and contributed to complications that ultimately caused her kidneys to fail. She had to be put on dialysis for two years before she was able to receive a kidney transplant in 2006.
Doctors also had to remove the burned portion of her small intestine, leaving her with just three functioning feet of her bowel. Diagnosed with short bowel syndrome (SBS), Lydia started to experience dramatic weight loss because her body could no longer absorb adequate nutrition. At 72 pounds, she was emaciated and unable to regain any weight. She became home-bound.
“I felt deeply frustrated,” Lydia said. “After beating a life-threatening cancer, I still had no strength or energy. I decided it was time to take some action to see what could make me better.”
In 2006, Lydia was introduced to Option Care by her attending physician and put on total parenteral nutrition (TPN), which gives her the nutrition she needs through intravenous delivery.
“TPN made an immediate difference in my overall health,” Lydia said. “I finally started to feel like myself again.”
Lydia and her husband are registered nurses so they are able to handle her TPN treatments and labs from home, self-infusing five days a week for nine hours at night. Lydia works closely with her care team at Option Care to receive additional antibiotics when she needs them. They also coordinate directly with her physicians to communicate any changes in her treatment.
“After many years with Option Care as my infusion provider, I’ve developed a close relationship with my care team and we’ve gotten to know each other on a personal level,” Lydia said. “You can tell that they care about what is going on with me and not just my medical health. I have complete confidence in their abilities to provide me with the best care possible.”
As a grateful cancer survivor, Lydia is thriving thanks to TPN. She credits her involvement with Option Care as enabling her to regain a near normal life. She is now able to visit her grandchildren who live six and a half hours away as well as escape the cold Minnesota winters for vacations in Florida and Arizona. Option Care supports Lydia by working with her to ensure she has access to necessary medications while she’s traveling.
“I can get out and get back a little bit of my life that I had before,” Lydia said. “It’s important to spend your energy on trying to get yourself better. Option Care home infusion helps me do that.”

Нутритивная поддержка
PHOENIX, March 21, 2019 — Clinical interventions provided by a nutrition support team can prevent hospital readmission in patients with short bowel syndrome (SBS) receiving home parenteral nutrition (PN), saving millions in costs annually, suggests a study[*]Englert M, Stodola K. Proactive Interventions by Nutrition Support Clinicians in Patients with Short Bowel Syndrome (SBS) on Home Parenteral Nutrition (HPN) Results in Decreased Hospitalizations and Improved Financial Outcomes. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. by Option Care Enterprises, Inc. ( “Option Care”), the nation’s leading provider of home and alternate site infusion therapy services. The research is being presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference and was chosen as an Abstract of Distinction.
Among SBS patients receiving home PN provided intravenously (IV), dehydration is a common cause of hospital readmission, with an average three-day length of stay. In the study, the nutrition support team — including a dietitian, nurse and pharmacist — made recommendations (interventions) to adjust the home PN volume based on the weekly monitoring of patients’ hydration status through reviewing laboratory values and conducting nutrition assessments.
“Home nutrition patients on PN with SBS need to be observed closely the first month to prevent dehydration and making appropriate adjustments to the home PN volume is essential,” said Mary Englert, MS, RD, CSO, LDN, CNSC, Area Lead, Nutrition Support Dietitian at Option Care and lead author of the study. “Every intervention decreases the likelihood of the patient being readmitted to the hospital and this study highlights the value of a nutrition team in providing clinical monitoring and nutrition support, which leads to improved patient care and significant cost savings.”
The study included 116 patients with SBS who received home PN after being discharged from the hospital. The Registered Dietitian-led nutrition support team provided ongoing evaluation by reviewing labs weekly and conducting a thorough nutrition assessment, recommending adjustments to the volume of PN when indicated for a total of 63 proactive interventions during the four-week review period. The most common reasons for home PN volume adjustments were: to meet the patient’s estimated fluid needs (56 percent); lab values reflecting dehydration (22 percent) and increased gastrointestinal output (22 percent).
Only 14 of the study patients were readmitted to the hospital within two weeks of discharge, none resulting from dehydration. Readmissions were due to: abscess/infection not related to PN (35.7 percent); line infection/replacement (21.4 percent); bowel obstruction (14.3 percent) and nausea/vomiting, feeding tube replacement, chest pain and unknown (7.1 percent each).
The researchers determined the interventions correlated to 189 hospital days prevented and $378,000 in costs saved in one month. Projected over one year that equates to 2,268 hospital days prevented and over $4.5 million in savings.
Also presented at ASPEN:
In another Option Care study[*]Hughey M, Corey B. Early Clinical Intervention Increases Compliance and Decreases Unnecessary Discontinuation in SBS Patients treated with Teduglutide. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. presented at ASPEN, 162 SBS patients were proactively screened for appropriate dosing before receiving teduglutide, which helps increase fluid and nutrient absorption resulting in decreased dependence on Parenteral Support. The clinical intervention resulted in recommended reductions to the prescribed dose in 64 of the patients (40 percent), half of which were based on impaired kidney function. Ensuring patients receive the appropriate dose reduces potential therapy complications including fluid overload, worsening kidney function and premature therapy discontinuation.
О компании Option Care
Option Care Enterprises, Inc. (Option Care) is the nation’s leading and most trusted provider of home and alternate site infusion therapy services. Holding accreditations from industry quality organizations ACHC, PCAB, ASHP and URAC,[*]Accreditation Commission for Health Care (ACHC), Pharmacy Compounding Accreditation Board (PCAB), American Society of Health-System Pharmacists (ASHP) and URAC the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature infusion services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.

Нутритивная поддержка
По данным исследования Option Care пациентам часто выписывают домашнее питание, которое не отвечает их потребностям
По данным исследования, представленного на Неделе клинического питания, без коррекции курс может привести к избыточности или недостаточности питания, проблемам со здоровьем и лишним расходам.
 ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
Исследователи Option Care выяснили, что назначаемая при выписке из больницы парентеральная (внутривенная) нутритивная поддержка на дому (ППД) не отвечает потребностям пациентов в одном из четырех случаев. И хотя потребности в питательных веществах чаще удовлетворялись при энтеральной (зондовой) нутритивной терапии на дому (ЭПД), 38% назначений не учитывали потребность в жидкости (поддержание водного баланса в организме). Сертифицированные диетологи Option Care проверяли все назначения, проводили оценку нутритивного статуса при переводе пациентов на домашний уход и при необходимости давали рекомендации по изменению назначения на основании лабораторных результатов анализов пациента, уровня активности и в целом состояния пациента.
“Nutrition support is complex and quality patient care provided in the home setting requires close collaboration between referring clinicians and a qualified home nutrition support team that has nutrition support expertise, including a registered dietitian, pharmacist and nurse,” said Noreen Luszcz, RD, MBA, CNSC, lead author of the study and nutrition program director for Option Care. “When a patient leaves the hospital, it is vital that the home infusion dietitian complete a nutrition assessment to ensure the order follows A.S.P.E.N. guidelines and the patient’s current needs are being met.”
Избыточность питания может привести к нарушениям обмена веществ и вызвать избыточный набор веса, не говоря уже об увеличении стоимости лечения вследствие использования большего объема питательных веществ, чем требуется. Недоедающие пациенты могут наоборот иметь недостаточный вес, их выздоровление может затянуться.
В исследовании, названном Американским обществом парентерального и энтерального питания (A.S.P.E.N.) лучшим стендом на Неделе клинического питания за качество и инновационный подход, был проведен анализ назначений нутритивной поддержки среди 187 пациентов на ППД и 349 пациентов на ЭПД, выписанных из больниц, где не было специально обученной команды нутритивной поддержки, которая могла бы скорректировать назначение.
Исследователи выяснили, что для 187 пациентов Option Care на ППД первоначальное назначение не соответствовало реальным потребностям пациентов в среднем 23% времени терапии. Они посчитали, что:
- у 41 пациента (22%) не соответствовал объем потребляемой жидкости;
- у 48 пациентов (26%) не соответствовал объем поступающих аминокислот (белков);
- у 39 пациентов (21%) не соответствовал объем поступающей декстрозы (углеводов);
- у 34 пациентов (18%) не соответствовал объем поступающих липидов (жиров), и
- у 51 пациента (27%) не соответствовал общий объем поступающих калорий.
Кроме того, 24 пациентам (13%) ошибочно назначили ППД, хотя им должны были назначить другие менее дорогостоящие способы питания, например, ЭПД и/или оральный прием. ППД необходимо назначать только пациентам, желудочно-кишечный тракт которых не в состоянии нормально переваривать и всасывать питательные вещества. Чаще всего нутритивную поддержку назначали терапевты (29%) и гастроэнтерологи (19%).
Что касается белка, первоначальное назначение, которое выписывали пациентам, вело к избыточности питания 48% времени терапии и к недостаточности питания 52% времени терапии. В остальных категориях пациенты с еще большей вероятностью получали первоначальное назначение, которое вело к недостаточному питанию. Исследователи оценили, что средний объем избыточно назначенного белка привел бы к дополнительным расходам в сумме $179 837 на пациента, получающего ППД в течение 90 дней, что составляет среднюю продолжительность терапии. Они посчитали, что если скорректировать потребление белка всего лишь в 12% назначений ППД, то можно добиться экономии для системы здравоохранения на сумму $5,2 миллиона.
По результатам оценки первоначального назначения исследователи определили, что из 349 пациентов Option Care на ЭПД:
- 133 пациентам (38%) не было назначено промывание водой (и следовательно, пациенты не получали достаточно жидкости);
- 15 пациентам (4%) были назначены смеси, не подходившие для их заболевания;
- 10 пациентов (2%) получали избыточное питание; и
- 18 пациентов (5%) получали недостаточное питание.
В исследовании указывается, что целый ряд факторов может привести к тому, что после выписки из клиники пациент может получать рекомендации, не отвечающие его потребностям. Схема питания, как правило, прописывается лечащим врачом, который может не иметь достаточных знаний о питании и не опирается на квалифицированную команду специалистов по нутритивной поддержке, включая сертифицированных диетологов, медработников и фармацевтов. Кроме того, потребности в питании со временем меняются. Пациенту при остром повреждении может требоваться больше белков для выздоровления, но потребность в них может снизиться к моменту выписки пациента из стационара. Если назначенная схема не корректируется, пациент может получить недостаточное или избыточное количество белков, которые со временем будут только накапливаться. И наконец, для назначения пациенту нутритивной поддержки на дому (особенно по программе Medicare) требуется провести тщательную диагностику, что в клиниках не всегда выполняется.
В программе нутритивной поддержки Option Care работают специалисты из разных областей, включая специалистов инфузионной терапии, фармацевтов и диетологов, специализирующихся на нутритивной поддержке, которые тесно взаимодействуют с лечащим врачом, чтобы обеспечить высочайший уровень ухода для пациентов, получающих парентеральное и энтеральное питание на дому. В каждом нашем филиале по всей стране работают сертифицированные диетологи.
Пациентам назначается парентеральное или энтеральное питание на дому по причине того, что они не получают необходимых питательных веществ перорально в связи с такими заболеваниями, как рак, инсульт, нарушения работы ЖКТ или осложнения после оперативных вмешательств. И хотя оба вида терапии могут временно осуществляться в больничных условиях, почти 40 000 пациентов в год парентеральное питание и 344 000 пациентов получают энтеральное питание безопасно и с меньшими затратами на дому, не подвергаясь риску заражения внутрибольничными инфекциями и возвращаясь к работе и активной жизни. Хотя некоторые пациенты проходят данные виды терапии в течение короткого срока, многим пациентам необходимо проходить их в течение длительного периода времени, а некоторым такая терапия необходима на протяжении всей жизни.
О компании Option Care
Option Care Enterprises, Inc. (Option Care) является одним из крупнейших и самых надежных в стране поставщиков услуг инфузионной терапии на дому или в альтернативных условиях лечения. Компания является лидером в отрасли и имеет почти 40-летний опыт лечения пациентов в соответствии с их индивидуальными потребностями. Уникальная программа Home Infusion Plus компании Option Care включает в себя клиническое применение лекарственной инфузионной терапии, сестринский уход и координацию оказания медицинских услуг. Многопрофильные специалисты Option Care, в том числе более 1 800 клинических специалистов, включая фармацевтов, медсестер и диетологов, могут проводить процедуры инфузионной терапии на дому практически для всех пациентов в США, которые нуждаются в лечении сложных и хронических заболеваний. Дополнительную информацию можно получить на сайте www.OptionCare.com.

Нутритивная поддержка
Many Home Parenteral Nutrition Patients Denied Medicare Reimbursement Несмотря на получение A.S.P.E.N. Лечение в соответствии с нормами
Исследование Option Care, подтверждающее важность покрытия лечения страховкой
 ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
Исследователи позволили выяснить, что более половины пациентов, получающих парентеральное питание на дому (внутривенно), лечение которых соответствует рекомендациям Американского общества парентерального и энтерального питания, не отвечают критериям страхового покрытия по программе Medicare. Такие результаты указывают на то, что критерии для оплаты парентерального питания на дому в Medicare устарели, в том числе это касается диагностических средств недостаточности питания, которые не отражают действующие рекомендации по уходу за такими пациентами.
“HPN is an expensive therapy and understandably Medicare wants to ensure that patients require that level of nutrition,” said Natalie S. Tu, RD, lead author of the study and clinical nutrition support dietitian for Option Care. “However, many malnourished patients have a clear need for HPN but don’t qualify for Medicare coverage. Care team members — including doctors and dietitians — need to diligently document the patient’s need in an attempt to secure Medicare coverage.”
In some cases, appeals providing additional documentation of need may be successful in securing coverage for patients initially denied by Medicare. Medicare patients who don’t qualify for coverage pay out of pocket costs which can be up to $250 a day and are prohibitive for many people. The average length of therapy for Option Care HPN patients is three months.[*] Option Care data on file.Patients who have supplemental insurance may be partially covered, but will be required to pay a daily deductible, which also adds up.
На данный момент почти 20 процентов пациентов Option Care на ППД обслуживаются по программе Medicare. И их количество продолжает расти по мере старения населения, а значит, возникает острая необходимость согласовать политику покрытия расходов Medicare с рекомендациями A.S.P.E.N., считает Ту.
За качество и инновационный подход исследование Option Care было названо лучшей научной работой Недели клинического питания A.S.P.E.N. Исследователи проанализировали 142 пациентов на ППД и определили, что 49 пациентов (35%) отвечают квалификационным критериям для прохождения ППД по программе Medicare, 56 пациентов (39%) не отвечают квалификационным критериям, а 37 пациентов (26%) находятся в подвешенном состоянии, так как квалификационный процесс был прерван или не завершен. Из 56 пациентов, не попадающих под критерии Medicare, 31 пациент (55%) не отвечает параметрам, установленным в руководстве Американского общества парентерального и энтерального питания.
Пациентам назначалось ППД по причине того, что они не получают необходимых питательных веществ перорально или посредством зонда (энтерального питания) в связи с такими заболеваниями, как рак, инсульт, нарушения работы ЖКТ или осложнения после оперативных вмешательств. И хотя ППД может осуществляться в больничных условиях, почти 40 000 пациентов в год проходят нутритивную терапию безопасно и с меньшими затратами на дому, не подвергаясь риску заражения внутрибольничными инфекциями и возвращаясь к работе и активной жизни.
В программе нутритивной поддержки Option Care работают специалисты из разных областей, включая специалистов инфузионной терапии, фармацевтов и диетологов, специализирующихся на нутритивной поддержке, которые тесно взаимодействуют с лечащим врачом, чтобы обеспечить высочайший уровень ухода для пациентов, получающих нутритивную поддержку на дому. В каждом нашем филиале по всей стране работают сертифицированные диетологи.
О компании Option Care
Option Care Enterprises, Inc. (Option Care) is one of the nation’s largest and most trusted providers of home and alternate treatment site infusion services. An industry leader, the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature Home Infusion Plus services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide home infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.
# # #